This past Friday was match day; a big moment in every doctor’s career. As usual, the AAFP put out an article with statistics on how many students matched into family medicine. As long as I’ve been following for the last five years, the articles are usually spun in a very positive light, highlighting the increased number of applicants into family medicine every year. What they don’t like to address is the continued decline of US MD applicants into the specialty, and the relative decrease in the number of people applying. The solutions they propose not only do nothing, but it may exacerbate the problem long-term.
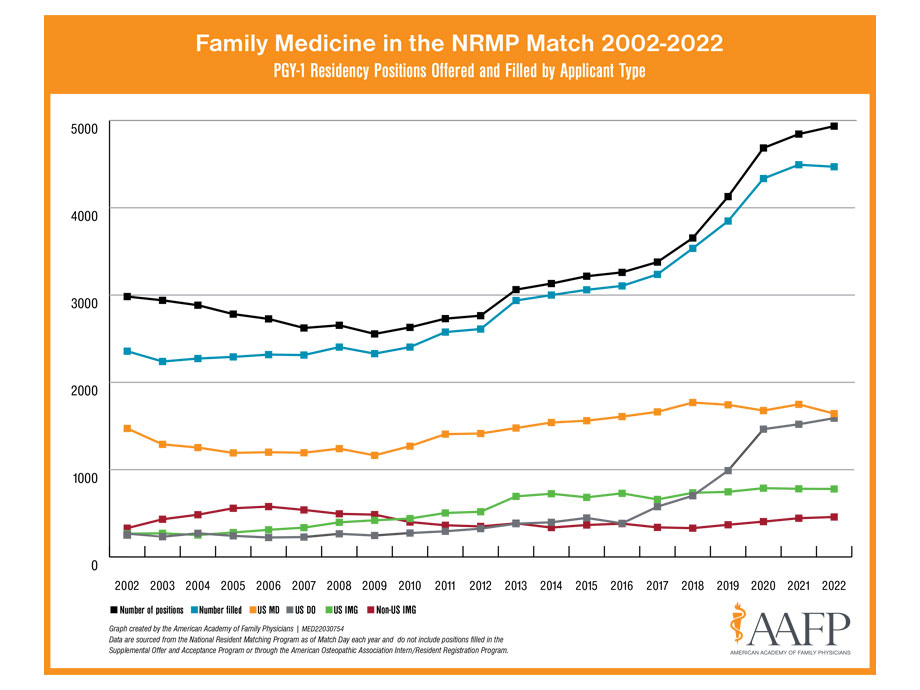
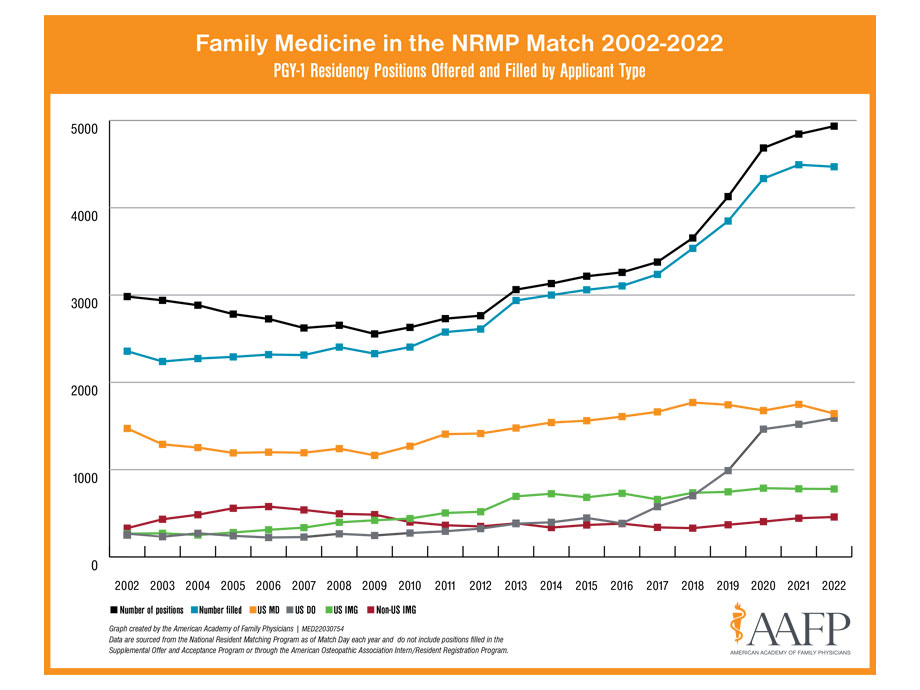
2018, the year I graduated medical school, was the last year that saw an increase in the number of US MDs applying to family medicine in a meaningful way. Last year, there was a small glimmer of hope when the specialty saw an increase of 66 students nationwide applying to family medicine, reversing a three-year trend of decline. This year, however, the decline erased last year’s increase and continued the worsening downward trend with 68 fewer US MD students matching into family medicine than last year. Currently, the specialty has been buoyed by a rapid rise in osteopathic schools pushing primary care in 2018-2019, but plateauing from 2020-2022. The AAFP article reports the percentage of DO students has matching into family medicine has actually been declining.
As the numbers of interested applicants plateau and decline, there is a push on many fronts to increase the number of primary care spots. Back when I was in medical school, I joined the state medical society in pushing some of these efforts. Since that time, I’ve realized the detrimental effects of doing so. Right now, the fundamental problem with family medicine is that nobody wants to do it. In other words, the perceived value by medical students of the specialty is very low. Who can blame them? When they are on their family medicine rotations in third year, they see burnt out doctors who are rushing from room to room. To increase the quantity of something with low value, lowers the value even more. What’s happening right now is basically the same thing as hyperinflation in Germany post World War I where people carried money in wheelbarrows to pay for basic necessities. The push for more primary care residency spots needs to stop.
With the increased number of spots and decreased number of applicants, more spaces are available for the SOAP. While the SOAP is a great opportunity for people who weren’t able to match into their top spots, it does create a problem when a specialty becomes the safety net. People who SOAP into family medicine, aside for the people who wanted to do family medicine all along and weren’t able to get into their preferred programs, usually are people who wanted to do something more competitive and otherwise couldn’t get in. Some of these individuals may eventually go on to have a great career in primary care, but a good number of these physicians begin their careers angry and upset, leading to an earlier chance of burnout. Not to mention, a portion of these individuals will also be actively trying to apply to their specialty of choice within the next year, leaving their programs potentially with open spots.
At the end of 2018, the AAFP launched the 25 x 2030 initiative, a goal to have 25% of US MD students applying to family medicine. At the start of that initiative, the number and percentage of US MD students matching into family medicine have decreased year over year, with just over 8% of US MD students applying into family medicine this year down from around 12% at the time of the initiative. Unless fundamental changes are made to how family medicine doctors are able to practice and get paid, there will be no increase in student interest in the field. DPC is the only primary care practice model so far which has captured the interest of medical students and gives family medicine a fighting chance to increase its imprint on the overall US healthcare system. Now more than ever, DPC doctors need to engage with their local medical schools by way of student shadowing, lunch lectures, and/or third-year rotations, in order to inspire and recruit the next generation of doctors into helping us fix and rebuild the primary care system.