

Originally published with Dr. Paulius Mui, MD
Terminology
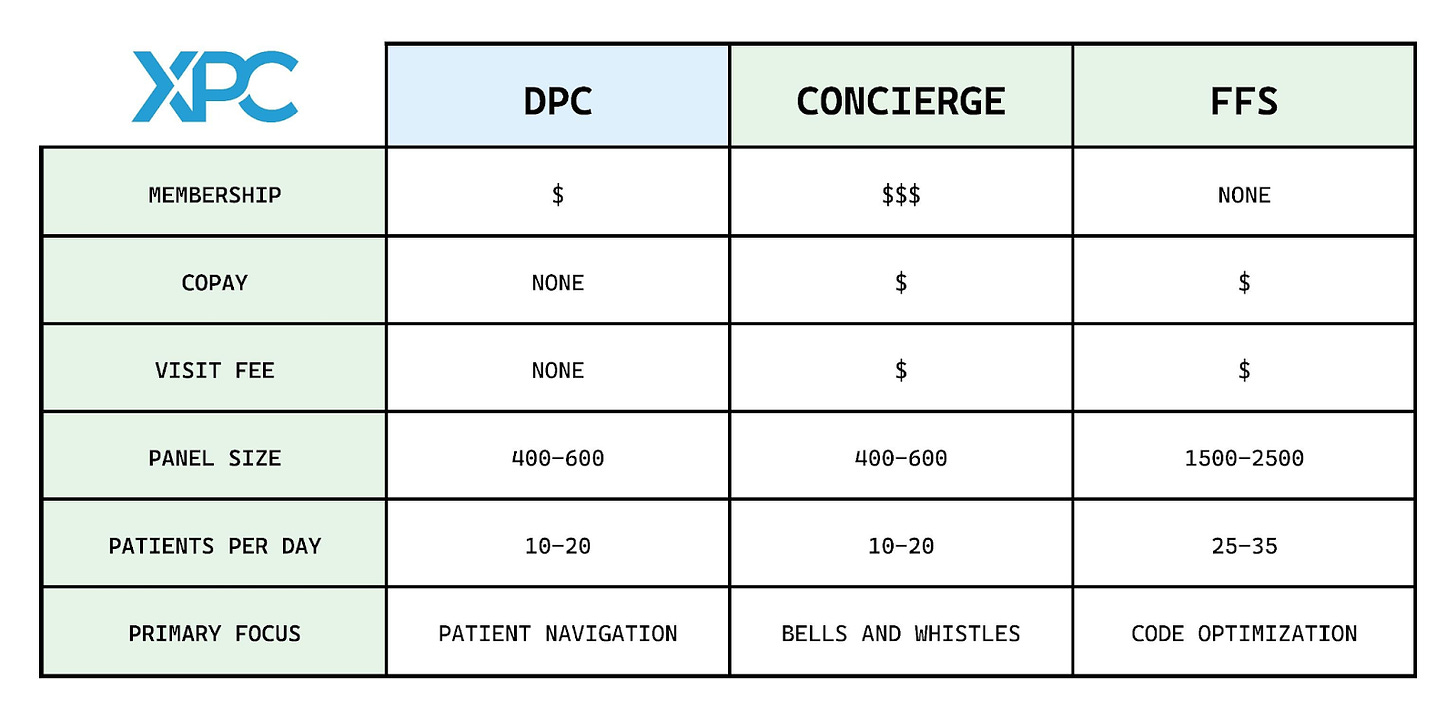
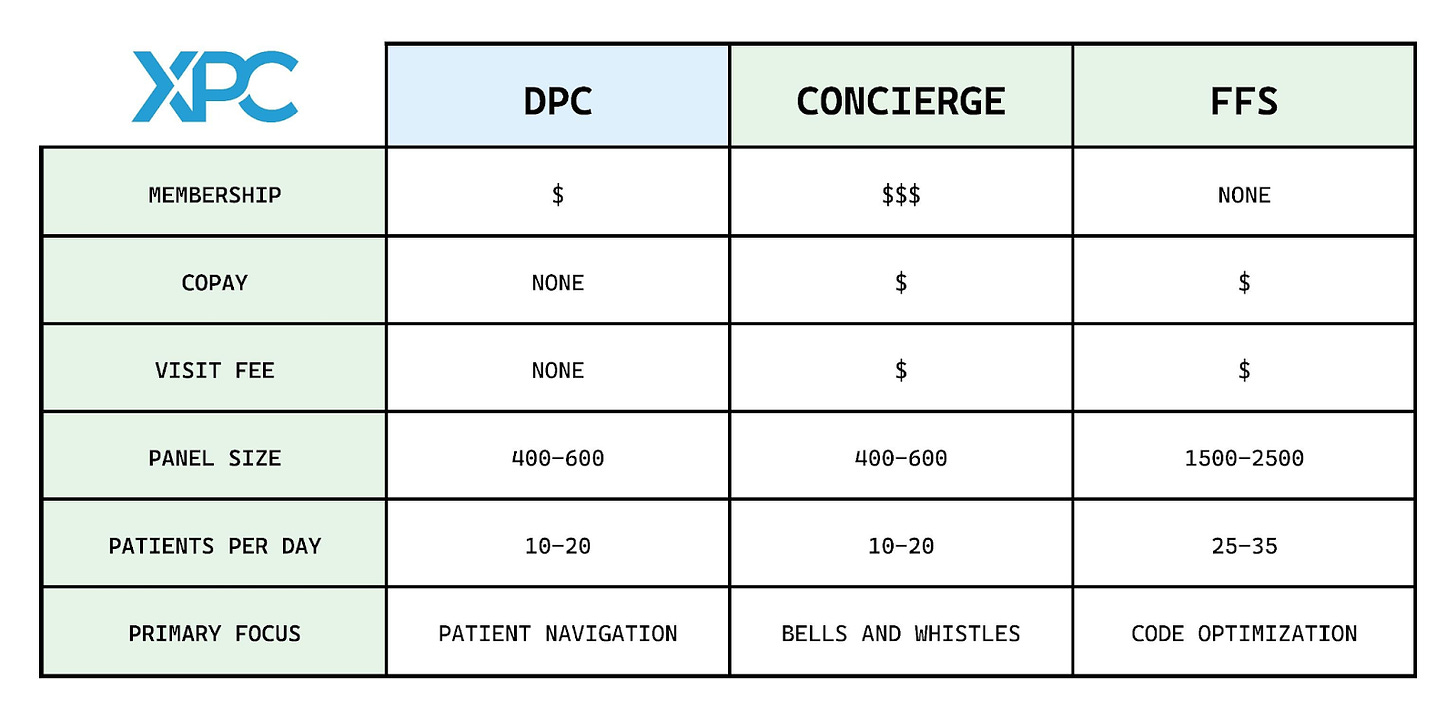
Understanding Direct Primary Care (DPC) begins with having consensus on what it means, not just for scholarly or marketing purposes, but also for legal implications as outlined by Dr. Phil Eskew: “1) charge a periodic fee. 2) not bill any third parties on a fee for service basis, and. 3) any per visit charge must be less than the monthly equivalent of the period fee.”
More terms to be aware of that may be misunderstood:
- Pure DPC = membership fees only, no insurance.
- Fee-for-service (FFS) = no membership fees, only bill insurance. If a patient doesn’t have insurance, then they have to pay out-of-pocket for medical services each time.
- Hybrid = one portion of patients pays only monthly membership fees while a different portion of patients are billed only through insurance (e.g. Rockwell Physicians). This can also be a transient state when practices are transitioning from FFS to pure DPC.
- Concierge = double-dipping in membership fees and insurance billing (e.g. MDVIP). Some DPC practices market themselves as concierge practices despite not taking any insurance to associate with high-touch experience.
DPC features
Applies to traditional brick-and-mortar practices.
- Smaller panel of patients, as low as 200 to 1200 per clinician (traditional panel size is about 3000 patients)
- Longer visit times 30-60 minutes or more
- Routinely use telehealth and text-based care
- Health system advocacy and navigation via discounted lab and imaging prices. Helping find cash pay specialists or using in house e-consult services.
Mappers
The DPC Frontier mapper has largely been considered the go to mapper. However, the mapper requires self reporting and exists more as a platform to display practices rather than an actively managed product, meaning there are no accuracy checks or quality control. The Alliance mapper only includes members of the DPC Alliance. Since health shares partner with DPC practices, the health shares have developed their own mappers for their members (e.g. Sedera, Zion HealthShare).


DPC origin story
Dr. Garrison Bliss is largely credited with starting the first DPC practice in 1997 in Seattle, Washington. During the first few years, Dr. Bliss fought with the then Insurance Commissioner of Washington state over whether or not his new model of practice constituted an insurance product. He eventually won that battle and went on to found Qliance, a multi-clinic DPC practice which famously piloted seeing Washington Medicaid patients on a per member per month basis. Jeff Bezos and Michael Dell were notable investors. Qliance ended in fiery failure for a number of complicated reasons. Dr. Bliss also founded the DPC Coalition, a lobbying organization, to help advance DPC legislation at the state and federal level and coined the term “direct primary care” for policy discussions. Wins for the organization include DPC language in the Affordable Care Act as well as favorable DPC legislationin a majority of states.
Other physicians independently created insurance-free practices in the early 2000s, and there was some convergent evolution with many physicians making their own DPC practices, like Dr. Bliss did, without previously hearing about the model. These physicians met at concierge conferences back in the day and eventually became some of the original members of the DPC Coalition. In 2012, FMEC spearheaded the first DPC summit and in 2018, the DPC Alliance formed.
Since independent physicians created the DPC model, most physicians feel the independent, small practice embodies the true spirit of DPC. As the DPC model grows and changes, these physicians believe new entrants, especially corporate and Virtual Primary Care, do not truly reflect the core philosophy of DPC and prefer to refer to them as DINOs (DPC In Name Only). Interestingly enough though, many of the corporate entities who do subscription model primary care do not generally call themselves DPC.Subscribe
Who is DPC?
We categorize the DPC landscape based on customer bases. In the retail model (B2C), memberships are sold directly to patients and can be led by individuals or corporations. In the employer model (B2B), memberships are sold to employers who offer DPC as a benefit to their employees. Both of these models can be led either by individual-owned practice networks or large corporations. DPC practices range in size from tiny to massive.
- Micro-practices (e.g. Defiant Direct Primary Care, EuDoc)
- Multi-clinician groups (e.g. Antioch Med, Direct Access)
- DPC physician networks (e.g. Nextera Healthcare, Primary Health Partners)
- Corporate (e.g. Everside Health, Crossover Health).
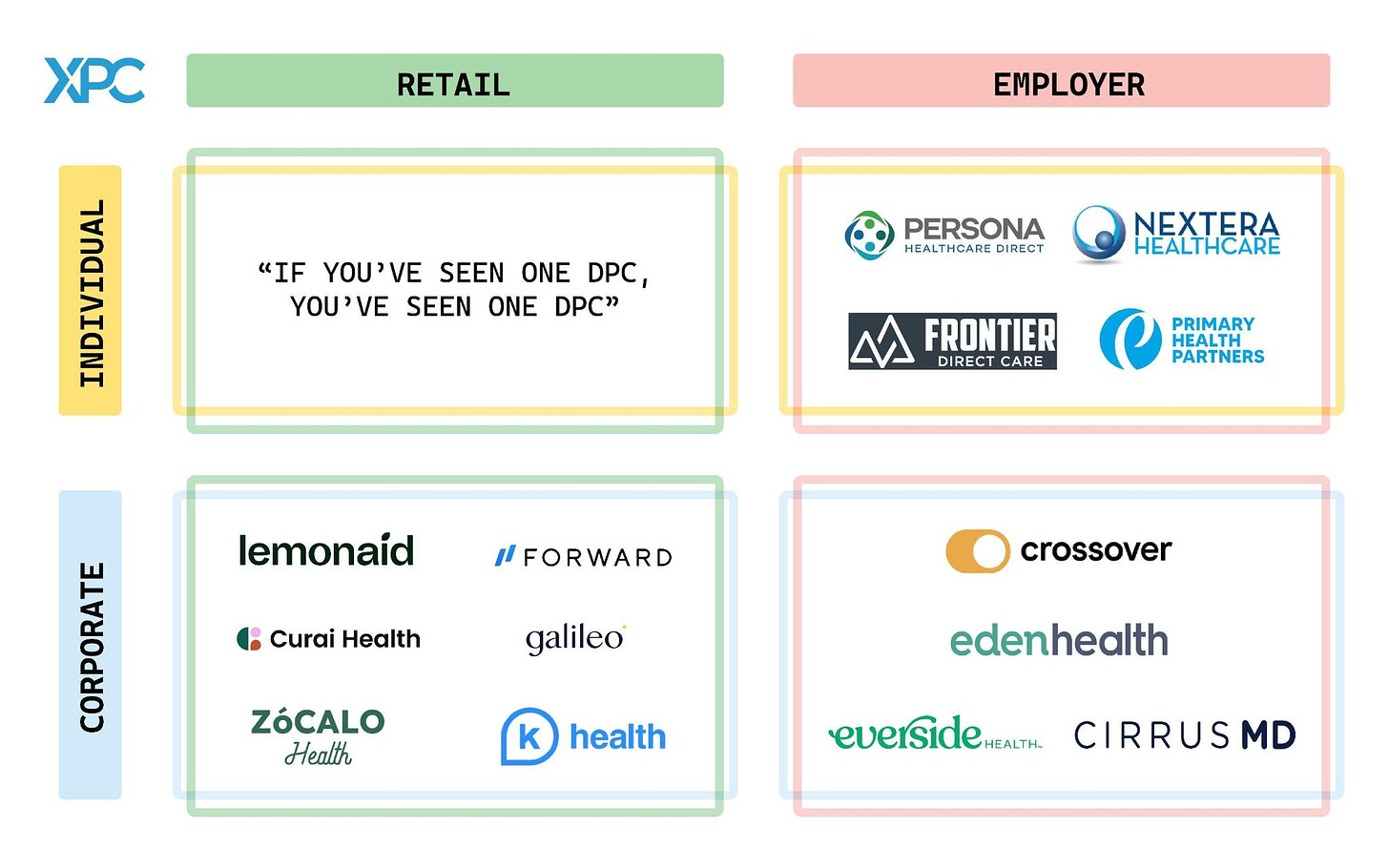
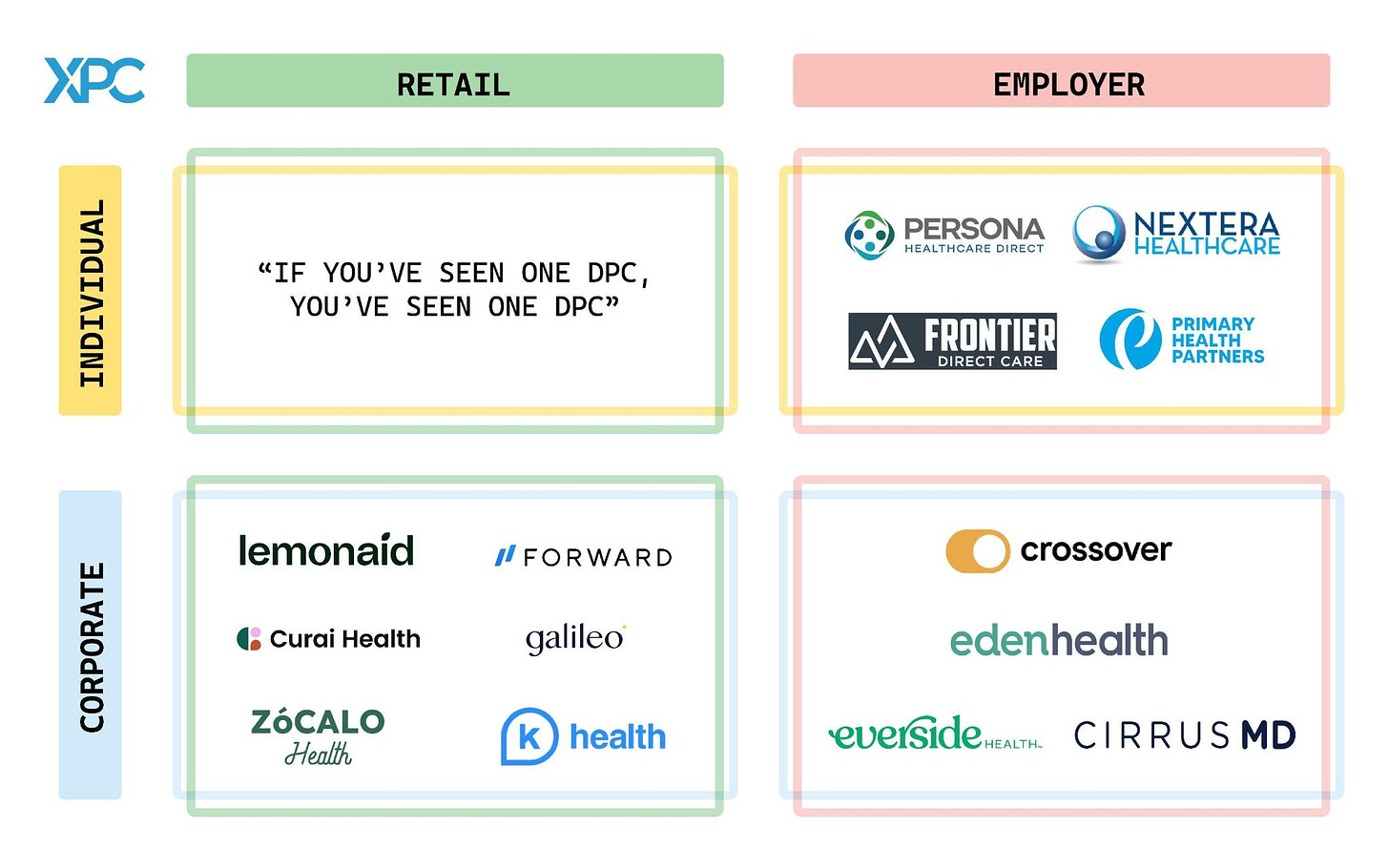
Individual-led retail practices
Practices founded by independent physicians, usually family medicine trained, range from micro-practices to multi-clinician practices which generally remain in their geographic location. A few of these are virtual with house calls, but the vast majority are traditional brick-and-mortar practices. There is a saying “if you’ve seen one DPC, you’ve seen one DPC.” Every clinician brings a unique take on their practice. We illustrate a variety of niches within DPC practices.
- Lifestyle and wellness – Dr. Lifestyle Clinic
- Bilingual – Dandelion Health
- LGBTQIA+ – Seven Hills Family Medicine
- Pediatrics and Lactation – Bloom Pediatrics & Lactation
- Full Spectrum with Obstetrics – Antioch Med
- Emergency Medicine Led – Thrive Direct Care
- Hospitalist Led – Fischer Clinic
- High-End – Priority Physicians
- House Calls – My Happy Doctor
Corporation-led retail practices
Tech-forward approach with broader geographic reach than individual-led retail practices. Most founders are not physicians. Generally limited in scope and primarily virtual (e.g. not all offer physical exams or office-based procedures that are included in traditional brick-and-mortar DPC memberships). For example, K Health and Curai are purely text-based care. Some are also working with health plans (e.g. Galileo and United Healthcare). From a patient’s point of view, this arrangement shifts the perceived identity of primary care physician from an individual to a corporation “your PCP with the United Healthcare Virtual First plan will be Galileo Health, rather than an individual provider.” Needs of traditionally underserved communities have attracted new entrants like Zócalo Health, which is focusing on the Latino community. Lemonaid Health expanded on-demand single-problem offerings to include virtual primary care membership through a partnership with SteadyMD. Forward stands out from the batch because it has physical locations for in-person care in addition to virtual and text-based care on top of perks such as in-home phlebotomy and prescription delivery. Crossover Health does have a consumer-facing DPC option, but we’ll group them with employer practices which aligns with their dominant business model.
Individual-led employer practices
Some independent DPC practices have found success working with businesses. They generally start as single or multiple physician practices which then grow to larger networks as they obtain larger contracts. While many of these practices have multiple locations and a handful of physicians, their networks involve contracts with other independent DPC practices to handle higher numbers of employees across a larger geographic location. Self-funded and level funded employers have benefitted from DPC arrangements. These practices work with benefit advisors and/or third-party administrators (TPAs) to help land more business accounts.
Some examples include:
Corporate-led employer practices
On-site/near site companies have existed for a while and never historically were considered DPC. Several newer companies made specifically for employers use a per member/employee per month model which technically makes them fit the legal definition of DPC.
- The growth of Crossover Health (XO) was catalyzed by Apple and Facebook onsite clinic contracts. Acquiring Sherpaa in 2019 further expanded their virtual care reach. The interdisciplinary approach to care gives XO patients access to latest tech-enabled primary care coupled with behavioral health, physical therapy, health coaching, care navigation and more. Aetna Advanced Primary Health, a zero-dollar employee benefit, has emerged from a recent partnership with Aetna.
- Everside Health has over 300 clinics in more than 30 states with focus on serving employers and unions. The company started out as Paladina Health, which was part of DaVita, and grew by subsequent acquisitions of Activate Healthcare, Healthstat and R-Health.
- CirrusMD serves “deskless workers” in customer service and blue-collar industries through text-first virtual primary care with access to specialists.
- Eden Health has a presence in-person and virtually with experts in insurance benefit navigation alongside their multidisciplinary clinical teams.
Hint Health recently launched Hint Connect which seeks to obtain larger employers by contracting across individual-led DPC practices to create a vast network under one umbrella. Their model makes them a bit of an anomaly which doesn’t fit neatly into any of the categories.
Special mentions
- At the academic center level, Hopkins is trialing a DPC model for their employees at their primary care clinics. University of Houston announced a DPC clinic a year ago which has closed due to unclear and unpublicized reasons.
- One Medical’s core business model by volume is concierge. They charge a very low membership fee and bill insurance with every visit. The DPC parts of this company’s portfolio include Iora, which started as DPC before pivoting to Medicare Advantage (MA), and several employer based DPC practices, such as the individual employer DPC group PeakMed. Interestingly, One Medical makes 17x more revenue per member with the MA business line.
- A polarizing topic for physicians that cannot be ignored is the increase of nurse practitioners (e.g. Nice Healthcare) and physician assistants (e.g. Smartypants Medicine) in independent primary care practice.
How does DPC interact with health insurance?
DPC physicians believe primary care, as a routine, inexpensive service, does not need and should not need insurance coverage. Most will advocate for a DPC membership to be combined with a high deductible plan or an alternative product like a health share (e.g. Zion HealthShare) or CrowdHealth. Some companies, however, feel DPC can live in harmony with insurance, and can look like simple capitation plans which historically have had different incentives.
- Taro Health is a startup insurance company on the ACA marketplace which has DPC as its foundation. They pay negotiated membership fees for in-network PCPs which are all DPC practices. They also strive to significantly reduce additional administrative burden compared to the incumbent insurance companies.
- Flume Health has partnered with Frontier Direct Care, allowing Frontier to build out their own personalized health plan.
- Decent operates as both a professional employer organization (PEO) and a health insurance company, providing a full suite of services for employers. They also have DPC as a foundation for their primary care, and recently added One Medicallocations to their offering.
- North Carolina-based Healthgram pairs in-house expertise as a TPA with their DPC physicians to cut costs for employers.
Major hurdles
- Health Savings Account (HSA) – Despite multiple state laws and federal letters of clarification, the IRS still believes DPC practices are health plans. The HSA issue remains muddy with one faction claiming HSAs are allowable and encouraging their use with and for DPC payments, while others, fearing audit, caution against pairing the two. Ultimately, this is an extremely esoteric discussion at a high level and left mostly for lawyers and accountants to decide at the individual level.
- Medicare – Medicare does not allow opted-in physicians to charge cash prices to beneficiaries. Theoretically, none of the retail corporate DPC companies can engage the Medicare population because of this rule. Most mature DPC practices have physicians who have opted out of Medicare. A much smaller number of practices are hybrid with only billing Medicare alongside their DPC practice. Since Medicare recipients are often the best candidates for DPC, removing the requirement to bill Medicare would help younger DPC practices start seeing Medicare patients sooner. Some companies like Pearl Health are trying to make Medicare arrangements more DPC-like through direct contracting. In the employer space, there is a gray zone argument where since the employer pays the membership, Medicare beneficiaries can see non-opted out physicians as a benefit rather than a traditional doctor visit, bypassing the billing requirement.
DPC tech stack favorites
- EMR – AtlasMD, Elation, Cerbo, AeroDPC (recently acquired by Hint Health)
- Practice management – Hint Health (billing), Spruce (patient communication)
- eConsults – Thea Health, RubiconMD
- Clinical tools – ButterflyiQ (handheld ultrasound), SkinIO (AI skin screening), Smartheart (EKG)
… many more out there.
DPC communities
Physicians in the DPC community come to these virtual watering holes (Facebook groups) for support and guidance. These are intentionally very hard to find and join. Almost all are invite-only.
- DPC Docs – Core DPC group.
- Pediatricians who do DPC
- DPC Women
- Direct Primary Care Alliance Group
- Regional DPC groups
- Direct Primary Care – Public group. Questionable content.
Organizations
Notable reports
- Direct Primary Care: Evaluating a New Model of Delivery and Financing by Society of Actuaries (2020)
- Hint Health Trends Report (2022)
Media
- Blogs – DPC News, DPC Frontier
- Podcasts – My DPC Story (interview with Dr. Qiu), plenty of single episodes about DPC on various podcasts
Popular Books by and for physicians
- The Official Guide to Starting Your Own Direct Primary Care Practice by Doug Farrago, MD
- Slowing the Churn in Direct Primary Care by Doug Farrago, MD
- Magic, Pixie Dust, and Miracles by Shane Purcell, MD
- Medical Answers Now!: How Direct Primary Care Guarantees Fast Access to Your Doctor by Troy Burns, MD
- Startup DPC: How To Start And Grow Your Direct Primary Care Practice by Paul Thomas, MD
- Sparks Start Fires: A Guide for Dreamers Who Are Also Doctors by Julie Gunther, MD
Tools for starting DPC practices
Conferences
- DPC Summit – main gathering for physicians interested in pursuing DPC or are currently practicing or growing DPC
- Hint Summit – health tech with a DPC focus
- You Powered Benefits Symposium and Health Rosetta Summit – benefit advisor conferences with strong DPC presence
- Free Market Medical Association Annual Conference – cash pay (i.e., non-insurance) based medical services
Special thanks to Celia for helping put together the visuals.
Phenomenal job. Thanks for putting this together
Many thanks to Kenneth for his engaging and thorough discussion of the evolution of DPC. It thrills me to see how this movement has evolved since 1997 when Mitch Karton and I sent a letter to our patients announcing that we were going to charge a monthly fee that covered all of our services at Seattle Medical Associates. At the time I was seeking a simplification and redirection of our business model that would allow us to practice better more personal and less encumbered primary care medicine. At the time,we had no certainty about whether this had any chance of succeeding and we had no path to follow or guarantee of success. As it became clear that we had stumbled into an oasis in the enormously disfunctional world of American health care, I felt obligated to share this with as many PCPs and patients as I could. I had no way to know that the outcome of our growth would require the efforts of multiple book authors and 2 major historians (Phil Eskew and Kenneth Qiu – both of whom I had the pleasure of meeting while they were still in training) to catalog the remarkable route our movement has taken. I love to follow the consequences of this culture as I follow the lives of my children and grandchildren – enjoying your accomplishments and inventions, and avoiding the urge to micromanage this movement. I send everyone engaged in this effort my love and appreciation for everything you have done for your patients and your country by pursuing our common goals: better care of patients and more affordable higher quality care for every American.