How much evidence does it take to influence clinical behaviors? Or a career decision?
Recently, I have been preparing a CME lecture to be given this fall on “CVD Prevention.” A challenging issue has been the lack of prospective, randomized, placebo-controlled clinical trials to answer many of our questions. How low to drive LDL-C in very high-risk patients? Less than 70? Or less than 45? Do we continue to use LDL-C, or switch to apoB instead? When do we use a “calcium score” by CT for risk stratification? We have plenty of observational data to address these questions, but not perfect RCTs. And likely, we never will. Given that CVD takes a life in this country every 34 seconds, and often prematurely or without warning, this is not a trivial matter.
And just today, contrary to many other expert bodies including the American Academy of Pediatrics, the U.S. Preventive Services Task Force (USPSTF) issued their opinion that current evidence is “insufficient” to recommend screening for lipid disorders in children and adolescents aged 20 years or younger due to the lack of RCTs to support doing so. This is also not a trivial matter, as heterozygous familial hypercholesterolemia (FH) affects one in 250 individuals, causes severe premature atherosclerosis, and is treatable.
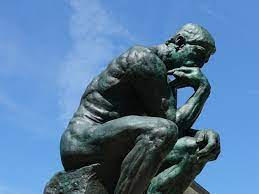
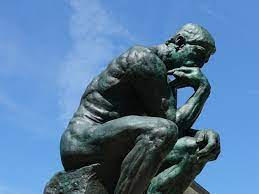
As Carl Sagan once said, “The absence of evidence is not evidence of absence.”
Very often in clinical medicine, especially when the stakes are high, we have to consider clinical strategies which are supported by science and evidence, tho not always the highest level of evidence. We should never ignore risks. But we should never summarily reject doing better because we lack overwhelming proof.
What does this have to do with DPC?
Physicians are unhappy. Burning out. How often I am not sure, but we do know, on average, one physician takes his or her own life every day in the U.S. A tragic statistic.
Patients too are unhappy. Just ask them.
What’s the solution?
We have enough evidence. We do not need an RCT to tell us. Yes, there have been DPC practices that have failed. But I have never talked to a DPC physician who longed to return to their previous fee-for-service life. And it is a rare patient who leaves a DPC practice because they dislike the concept.
Do we really need more evidence than that? I am sure there are those who cling to the status quo who would say so.
I am convinced we can do a better job better preventing CVD. I am also sure we can do better than subject physicians and patients to impersonal, assembly-line, insurance-dependent misery. DPC may not be perfect. But it’s far better than the norm. I don’t need a never-to-come RCT to tell me that.